Delhi | Kolkata
Bangalore | Chennai
Spine Surgery in India

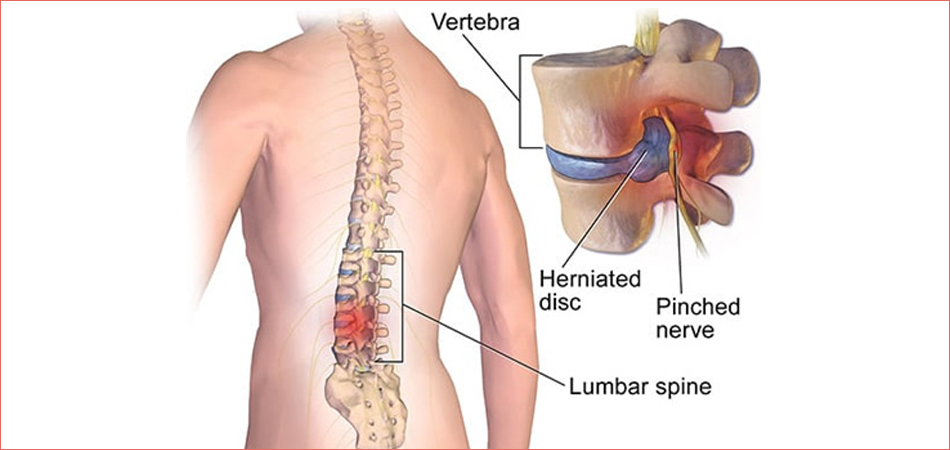
Aging, wrong body mechanics, shock and structural irregularities can injure your spine, leading to back pain and other indications such as leg pain and/or lack of feeling or even leg weakness. Chronic back pain is a disorder that generally needs a team of health professionals to diagnose and treat. If one is suffering from problems with back pain for any period of time, one may be wonder if spine surgery is the only viable treatment option. The vast majority of back complications can be remedied with non-surgical treatments—often referred to as non-surgical or conservative therapies. Sometimes, surgery is the only solution. Before thinking of surgery, consider getting estimations from several spine surgery experts. This investment of time and information assembly helps one make a reasonable treatment decision that will best support your lifestyle and preferred level of physical activity. Most pain in the lower back can be cured without surgery. Nonetheless, there are times when back surgery is a viable or needed option to treat serious musculoskeletal injuries or nerve compression. A pain management specialist can help you resolve whether surgery is a suitable choice after making sure you have exhausted all other possibilities.
Considering Back Surgery
The following conditions may be candidates for surgical treatment:
- • Herniated or ruptured disks, in which one or more of the disks that cushion the bones of the spine are injured
- • Spinal stenosis, a contraction of the spinal column that puts burden on the spinal cord and nerves
- • Spondylolisthesis, in which one or more bones in the spine slip out of position
- • Vertebral fractures caused by damage to the bones in the spine or by osteoporosis
- • Degenerative disk disease, or damage to spinal disks as a person gets older
In exceptional cases, back pain is caused by a tumour, an infection, or a nerve root problem called cauda equina syndrome. In these cases, it is recommended to conduct surgery right away to ease the pain and avert more problems.
Conservative non-surgical treatment
As with all non-emergency spinal surgeries, an experimental non-operative treatment, such as physical therapy, pain medication—preferably an anti-inflammatory, or bracing should be considered before surgery is seen as a viable option. The test period of conservative treatment differs, but six weeks to six months is the common timeframe.
Spine surgery may be endorsed if non-surgical treatment such as medications and physical therapy fails to relieve difficulties. Surgery is only considered in cases where the exact source of pain can be found—such as a herniated disc, scoliosis, or spinal stenosis.
Open surgery vs. minimally invasive spinal surgery
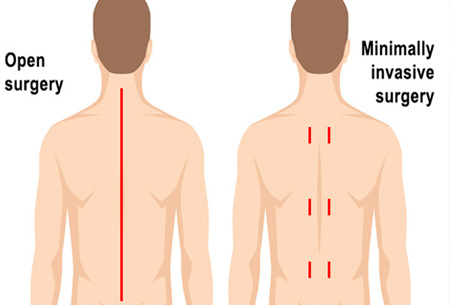
Conventionally, spine surgery is usually executed as open surgery. This involves opening the operative site with a long incision so the surgeon can view and access the spinal anatomy. However, technology has developed to the point where more spine conditions can be cured with minimally invasive techniques.
Because minimally invasive spine surgery (MISS), does not involve long incisions, open manipulation of the muscles and tissue surrounding the spine is circumvented, therefore, leading to shorter operative time. Generally, decreasing intraoperative (during surgery) manipulation of soft tissues ensures less postoperative pain and a quicker recovery.
Imaging during Spine Surgery

Computer-assisted image supervision allows surgeons to see the operative site in far better precision than traditional visualization methods. In addition, implants such as rods or screws can be introduced and positioned with a greater degree of exactitude than is generally accomplished with conventional procedures.
In computer-assisted image guidance, images taken preoperatively (before surgery) are fused with images acquired while the patient is in surgery, resulting in real-time views of the anatomical location and orientation of the operative site while the patient is in surgery. Preoperative computed tomography (CT) and intraoperative fluoroscopy (real-time x-ray) are usually used, as these enable surgeons to manoeuvre with a high level of accuracy and safety.

Spinal instrumentation
Examples of spinal instrumentation include plates, bone screws, rods, and interbody devices; although, there are other types of devices a surgeon may endorse in treatment of a spinal disorder. The reason for instrumentation is to stabilize or fix the spine in position until the fusion solidifies.
- • An interbody cage is a permanent prosthesis left in place to maintain the foraminal height (e.g., space between two vertebral bodies) and decompression following surgery.
- • Interspinous process devices (ISP) reduce the load on the facet joints, restore foraminal height, and provide stability in order to improve the clinical outcome of surgery. An advantage of an ISP is that it requires less exposure to place within the spine and therefore is a MISS procedure.
- • Pedicle screws help to hold the vertebral body in place until the fusion is complete.
Before Surgery
By the time one signs up for back surgery, the doctor probably has tried different forms of treatments to ease the back pain or lower body pain. While there are no assurances that the operation will provide respite, there are lots of preferences. Study as much as you can about back surgery before time. The more you know, the better choice you’ll make.
In your pre-surgery consultations with your medical team, it’s important to perfectly answer questions associated to your medical history, allergies, medication schedule, and lifestyle choices, as these can help the doctor understand the prospective surgery risks. Numerous factors can affect your risk for a surgical complication, such as:
- • General health
- • Age
- • Prior surgical experience
- • Existing medical conditions (such as diabetes)
- • Smoking status
- • Osteoporosis
Types of Surgery
Vertebroplasty and kyphoplasty:

These techniques are used to repair compression fractures of the vertebrae caused by osteoporosis. Both techniques include the injection of a glue-like bone cement that toughens and fortifies the bone.
Spinal laminectomy/spinal decompression: 
This is done when spinal stenosis causes a narrowing of the spinal canal that results in pain, discomfort or weakness. The surgeon eliminates the bony walls of the vertebrae and any bone spurs, targeting to open up the spinal column to eliminate pressure on the nerves.
Discectomy: 
This process is used to remove a disk when it has herniated and presses on a nerve root or the spinal cord. Laminectomy and discectomy are often executed together.
Foraminotomy: 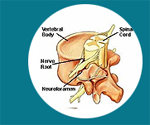
In this process, the surgeon expands the bony hole where a nerve root exits the spinal canal to prevent bulging disks or joints thickened with age from pressing on the nerve.
Nucleoplasty:
It is also called plasma disk decompression. This laser surgery uses radiofrequency energy to cure people with low back pain associated with a slightly herniated disk. The surgeon implants a needle into the disk. A plasma laser device is then implanted into the needle and the tip is heated, forming a field that vaporizes the tissue in the disk, reducing its size and dismissing pressure on the nerves.
Spinal fusion: ,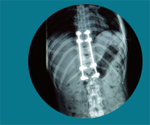
The surgeon removes the spinal disk between two or more vertebrae, then linked the adjacent vertebrae using bone grafts or metal devices supported by screws. Spinal fusion may end in some loss of flexibility in the spine and needs a long recovery period to permit the bone grafts to grow and join the vertebrae together
Artificial disk replacement: ,
This is thought of a substitute to spinal fusion for the treatment of people with severely damaged disks. The process comprises removal of the disk and its replacement by a synthetic disk that helps restore height and movement between the vertebrae.
Risks
Most people who get back surgery have marginal, if any, difficulties. That said, any operation has some sort of risk, including:
- • Reaction to anaesthesia or other drugs
- • Bleeding
- • Infection
- • Blood clots, for instance in your legs or lungs
- • Heart attack
- • Stroke
- • Herniated disk
- • Nerve damage, which can lead to weakness, paralysis, pain, sexual dysfunction, or loss of bowel or bladder control
The chances that something could go wrong go up for people with certain health situations. They also vary by type of surgery. Part of your surgeon's job is to classify potential difficulties. So talk it over before you head to the Operation room.
Considerations for Anaesthesia during Surgery
Back surgery will almost always be done under general anaesthesia. In addition to the typical risks associated with anaesthesia, there are risks associated with the patient lying face down on the surgical table. This position alters the body’s hemodynamics — that is, how blood flows through the body. The position also restricts the surgical team’s access to the patient’s airway. This requires extra care in the arranging of equipment, monitors, patient and anaesthesiologist. It is really important to have a physician anaesthesiologist in the operating room to make sure all is set up appropriately and to be able to take instant action in case anything goes wrong.
Post-Operative Recovery
Back surgery can cause a high level of post-operative discomfort. One should consider a different options for pain relief in the days and weeks after surgery. These possibilities should be discussed with a pain management specialist who can clarify the pros and cons of each choice or grouping of options, including their efficacy, possible side effects, potential for addiction and bearing on the recovery process.
Some factors to consider:
• Many of the options will encompass medications such as opioids, nonsteroidal anti-inflammatory drugs, corticosteroids and local anaesthetics. Occasionally more than one drug is taken. This multimodal therapy can develop pain control while limiting opioid use.
• Opioids should be used with care to avert addiction and cope with side effects, some of which can be dangerous.
• Alternative or matching methods of pain relief that do not involve medicines should be conferred.
Physician anaesthesiologists who specialize in pain management can work with the patient before and after surgery to develop a plan tailored to the situation, personal history and predilections. They will consult with the patient after surgery to conclude what is working and what is not, and they will correct the pain management treatment based on the level of pain the patient is suffering from.
Physician anaesthesiologists work with the physician team to estimate, monitor and oversee the care before, during and after surgery, providing anaesthesia, supporting the Anaesthesia Care Team and ensuring the patient’s utmost safety.
* Conditions Apply

